
Osteochondrosis is one of the most common diseases of the musculoskeletal system, manifested as a complex of certain dystrophic changes in the cartilage of the vertebrae, during which pathological discs are often involved. Intervertebral discs provide structures with flexibility and also allow movement of the human spine, i. e. , movement.
In osteochondrosis, there are a number of processes that cause degeneration in the vertebral discs, as a result of which they begin to lose their elasticity and reduce the degree of elasticity, and at this time the disc itself becomes quite flat. The distance between the two plates decreases while compressing nerve endings and blood vessels and causing severe pain. The site of compression of the nerve node begins to swell, leading to increased pain and even greater violation.
During the development of osteochondrosis, most of the muscle structures and organs of the body are involved in this pathological process. This is due to the fact that during maximal violation of the neurovascular bundle, blood circulation and movement of muscles and organs are disturbed. For example, the most common osteochondrosis is cervical osteochondrosis, which is accompanied by pain in the back of the head, nausea, dizziness, blurred vision, and often tinnitus. This disease has become quite "younger": a century ago, osteochondrosis was a disease of people of gerontological age, and today young people are susceptible to it.

The most vulnerable categories of people are those with severely impaired metabolism and hormonal levels in the body, and those with vascular-venous disorders. This is due to the fact that these diseases disrupt the oxygen supply to the plate. If proper, timely measures are not taken to heal, the edges of the affected intervertebral disc, which compress, anatomically extend beyond the boundaries of the spinal column and destroy the neurovascular bundles.
Because of this, the patient is at risk for developing a disc herniation. The main significant cause of osteochondrosis is the uneven distribution of the load on the spine, leading to the fact that the cartilage structure changes at points of excessive pressure. The nature of the disease depends on the stage and extent of damage to the affected plates. Intervertebral discs change as our hair progresses with age. Severe injuries or fractures of the spine can affect their function. Casual wear and certain types of vibrations can also accelerate spinal degeneration. In addition, evidence suggests that smoking increases the rate of spinal degeneration. Scientists have also found a link between family members, highlighting the role of genetics in how quickly changes occur.
The disease can be caused by several factors:
- injuries, bruises;
- spinal dystrophy;
- curvature and curvature of the spine;
- weight-lifting;
- long stay in one situation;
- metabolic disease;
- lack of trace elements and vitamins - manganese, magnesium, zinc and vitamins D and F;
- hereditary predisposition;
- physical overload;
- sedentary lifestyle;
- radiation background;
- freezing;
- congenital dystrophies;
- asymmetrical work of the muscles of the spine;
- stress, depression.
These causes of osteochondrosis are just assumptions by scientists, direct factors causing the disease that science has not yet found, and we are only talking about risk factors.
First perioddevelopment - characterized by early introduction of the intradiscular nucleus pulposus (adjacent to the dorsal part of the nucleus pulposus of the eccentric intervertebral disc).
In the second periodcharacterized by the appearance of spinal segment instability. Pathological substrates are represented by the fibrous core of the affected disc with degenerative processes of ascension and fragmentation of the posterior longitudinal ligament, with abnormal movements developing between the vertebrae.
Third periodthe development of the disease - complete damage to the intervertebral disc, with the appearance of a "herniated disc" - the displacement and exit of fragments of the nucleus pulposus outside the intervertebral space.
Once the disease has reached the third phase, the process of destruction is already irreversible and can lead to profound disability.
Types of osteochondrosis
The evolution of osteochondrosis is slow, with exacerbations of spinal injuries, exercise, weight bearing, and so on. The clinic depends on the location of the lesion.
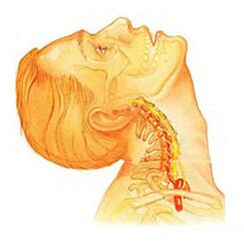
Osteochondrosis of the cervical spineits advanced forms have local and distant symptoms - with loud root dominance, i. e. , it contributes to the development of severe radical pain. Symptoms of cervical spine osteochondrosis are accompanied by varying degrees of dysfunction, sometimes manifested by abrupt restrictions on cervical spine and functional block mobility. The headache can be both pulling and paroxysmal in nature, with irradiation in the interscapular region or the shoulder area. During the acute period, patients are diagnosed with seizures of neck pain that prevent and restrict movement of the head and neck. In addition to severe discomfort, pain syndrome can be associated with dizziness, insomnia, pain, loss of appetite, depression, and eye and pharyngeal disease.

Chest osteochondrosis. . . Clinical manifestations are due to local lesions and destruction processes of the nerve root structure. Chest osteochondrosis has a pronounced pain syndrome that can have chronic or acute back pain such as chest discomfort and limited muscle contracture, all the way to right-verbal muscle atrophy. Chest pain can take diffuse, intercostal and neuralgic forms. The touch enhances the axial rotation of the vertebral body. The disorders correspond to the level of root irritation from Thl1 to Thl2 and may manifest as angina pectoris, which is reflected in dysfunctions of the liver and gastrointestinal tract. Disorders of the urogenital system and genital area are common. Patients note sensory disorders such as paraesthesia, with a significant decrease in surface and deep sensitivity.

Lumbar osteochondrosis. . . It is characterized by dysfunction of the abdominal reflexes and lower extremities. During the development of neurological disorders, muscle weakness of the legs and dysfunctions of the pelvic organs may occur. Osteopondrosis is characterized by the assessment of damage to the sitting process. The more advanced the stage of development of lumbar vertebral lesions, the shorter the patient can sit. Lumbar forms are characterized by chronic and acute back pain, paravertebral muscle spasm, and myofascial secondary syndrome. The pain radiates to the buttocks and posterior ilium.
Depending on the localization of the pathological process of osteochondrosis, the disease may lead to a violation of superficial sensitivity (tactile, thermal). Also characteristic are changes in reflexes (e. g. , lack of Achilles reflex), muscle atrophy, muscle tone disorders, autonomic disorders (pallor, redness of the skin, trophic changes in nails, hypothermia of the skin in the distal limbs), and sphincter dysfunction. dysfunctions.
Clinical picture
Diagnosticsbegins with a complete medical history and physical examination. The doctor asks questions about the symptoms, how the disease affects the patient’s daily activities. In addition, the practitioner is interested in positions and activities that emphasize or reduce the level of pain.
The doctor then examines the patient, checking the position and range of motion of the spine, thereby determining which movements are causing the pain. Skin sensitivity, muscle strength and reflexes are all tested. Based on your medical history and physical examination, your doctor will determine which techniques will help.
Radiography rarely aids diagnosis, with up to 30% of radiographic images showing abnormalities in the early stages of disease development.
However, if the symptoms are severe and the disease is already in the second or third stage, the picture will show defects in one or more intervertebral discs. Osteophytes can penetrate the vertebrae and joints.
If additional information is required, magnetic resonance imaging is prescribed. MR is used to view the soft tissues of the body. This is useful if the core of the fabric absorbs water or if there are cracks inside the plate. MRI can detect problems in other soft tissues, such as the nerves in the spine.
Discography can help with diagnosis. This test is performed with a contrast agent that is injected into one or more discs. Post-viewing the X-ray provides useful information about the condition of the discs.
Treatment of osteochondrosis, depending on the variety
Non-surgical treatment of osteochondrosis
Whenever possible, physicians prefer non-surgical treatment. In non-surgical treatment, the most important thing is to relieve pain and other discomfort so that the patient can continue to enjoy a comfortable standard of living as much as possible.
Doctors rarely prescribe bed rest for patients with osteochondrosis problems. Patients are encouraged to live in natural motion if the pain is not a problem. If symptoms are severe, several days of bed rest may be prescribed.
When the spine moves, an elastic belt is sometimes prescribed, which is worn for up to 2-4 days to avoid atrophy of the back muscles.
Osteopathic occupations provide significant relief in osteochondrosis.Osteopathic doctornot only does it diagnose a problem area, but it relieves pain in 1-2 doses, relieves the general condition of the body, and "tightens" the visceral organs.
Patients may be prescribed medications to treat their symptoms and to resume normal activities for a long time. If symptoms continue to limit the patient's activity, a traditional physician may recommend an epidural steroid injection.
Steroids are powerful anti-inflammatory drugs that help relieve pain and inflammation. Non-steroidal anti-inflammatory injections are injected into the space around the spinal roots of the spine. This place is called the epidural space. Some doctors administer the steroid alone. Most often, however, it is combined with other drugs. Basically, steroids are only prescribed when other medications are ineffective, but osteopathy almost always helps.
In addition, patients often work with physiotherapists. After assessing the patient’s condition, the therapist prescribes exercises to reduce symptoms. The workout program is designed to improve flexibility and is useful for training the abdominal and back muscles to move with the least amount of pain.
Surgery
People with osteochondrosis usually do not require surgical treatment. In fact, only 1-3% can be operated. Surgeons prescribe non-surgical treatment as a rehabilitation, namely craniosacral osteopathy, for at least 3 months before surgery is considered. If there are no results after 3 months of non-surgical treatment, there are only reasons that indicate surgery.
Basic surgical procedures
Discectomy
The purpose of the procedure is to partially or completely remove the disc in the lumbar region. Surgeons usually perform the operation through an incision in the lumbar region. Some of the discs should be removed before removing the disc herniation.
Today, surgery has mastered minimally invasive techniques that require only a small incision in the lumbar region. Proponents of the method claim it is safe. It is also believed that the procedure prevents scarring around nerves and joints and helps patients recover faster.
It merges
It is an intervention that combines two or more bones together to prevent wear on the ends of the bones and joints.
Rehabilitation
Your doctor may recommend that you see your doctor several times a week for 4-6 weeks. In some cases, patients need additional help.
The first year of treatment is needed to treat the symptoms. The therapist will work with you to find pain-relieving situations and movements. Heat, cold, ultrasound, and electrical stimulation may be prescribed to relieve pain and muscle cramps. Special forms of massage or soft tissue mobilization can also be used. These procedures help the patient to perform movements with ease.
Adjusting the treatment usually helps to restore the sensitivity of the spinal nerves and muscles, reduce pain, and improve mobility.
The main goal of therapy is to teach the patient how to manipulate to prevent future problems. The patient is offered a series of exercises to improve flexibility. The patient also receives a strategy to help with recurrent symptoms.
All people should study and consider all types of osteochondrosis to prevent this disease from developing in themselves and their loved ones. After all, treatment of destroyed vertebrae is impossible, with therapy aimed at relieving pain symptoms and achieving long-term remission. You should also remember a simple but effective rule:the best cure is prevention. . .
Prevention of osteochondrosis
Prevention is fairly simple - it’s a healthy diet, regular muscle activity, a daily morning warm-up, a healthy and active lifestyle, and a monthly visit.osteopathic occupationsfor the correction and removal of locomotor tensions. Adherence to these rules is enough to never face the problem mentioned above and avoid terrible symptoms and lifelong treatment.































